Alzheimer’s disease
•Dementia
is a syndrome characterized by progressive loss of previously acquired
cognitive skills including memory, language, insight, and judgment.
•Alzheimer's
disease accounts for the majority (50%
to 75%) of all cases of dementia.
•Approximately
10% of all persons over the age of 70 have significant memory loss, and in more
than half the cause is AD
EPIDEMIOLOGY & DEMOGRAPHICS
•INCIDENCE:
Risk doubles every 5 yr after the age of 65; above the age of 85th incidence
is about 8%.
•PREVALENCE:
Currently an estimated 4 million Americans have AD; 7% between the ages of 65
and 74, 53% between the ages of 75 and 84, and 40% over the age of 85.
•PREDOMINANT
SEX: Female
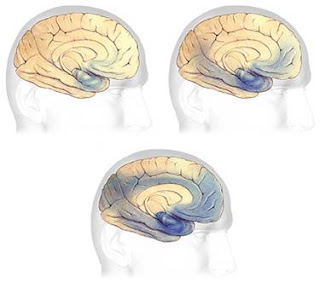
The Brain and Alzheimer’s Disease
Two major structural changes:
1.Neurofibrillary
tangles-Bundles
of twisted threads that are the product of collapsed neural structures (contain
abnormal forms of tau protein
2.Amyloid
plaques-Dense
deposits of deteriorated amyloid protein, surrounded by clumps of dead nerve and glial cells.

earliest and most severe degeneration is usually found
in the medial temporal lobe
: (entorhinal/perirhinal cortex hippocampus),
lateral
temporal cortex, nucleus basalis of Meynert
These images represent a cross-section of the brain as
seen from the front. The cross-section on the left represents a normal brain
and the one on the right represents a brain with Alzheimer's disease.In Alzheimer's disease,
there is an overall shrinkage of brain tissue. The grooves or
furrows in the brain, called sulci (plural of sulcus), are noticeably widened and there is shrinkage of the gyri (plural of gyrus), the well-developed
folds of the brain's outer layer. In addition, the ventricles, or chambers
within the brain that contain cerebrospinal fluid, are noticeably enlarged. In
the early stages of Alzheimer's disease, short-term memory begins to fade (see
box labeled ‘memory') when the cells in the hippocampus, which is part of the
limbic system, degenerate. The ability to perform routine tasks also declines.
As Alzheimer's disease spreads through the cerebral cortex (the outer layer of
the brain), judgment declines, emotional outbursts may occur and language is
impaired. As the disease progresses, more nerve cells die, leading to changes
in behavior, such as wandering and agitation. In the final stages of the
disease, people may lose the ability to recognize faces and communicate; they
normally cannot control bodily functions and require constant care. On average,
the disease lasts for 8 to 10 years, but individuals with Alzheimer’s can live
for up to 20 years.
Severe Alzheimer’s Disease
Several competing hypotheses:
Cholinergic hypothesis
-Caused by reduced synthesis of acetylcholine
-Destruction of these neurons causes disruptions in
distant neuronal networks (perception, memory, judgment)
Amyloid hypothesis
-Abnormal breakdown; buildup of amyloid beta deposits
-Damaged amyloid proteins build to toxic levels, causing call damage and
death
Tau hypothesis
-Caused by tau protein abnormalities
-Formation of neurofibrillary tangles
PHYSICAL FINDINGS & CLINICAL PRESENTATION
•Family member, not the
patient, often notes insidious memory impairment.
•Patients have difficulties
learning and retaining new information, handling complex tasks (e.g., balancing
the checkbook), and have impairments in reasoning, judgment, spatial ability,
and orientation (e.g., difficulty driving, getting lost away from home).
•Behavioral changes, such as mood
changes and apathy, may accompany memory impairment.
In later stages patients may develop agitation and psychosis.
DIAGNOSIS
•Diagnosis
is dependent on
clinical history, a thorough physical and neurologic examination, and use of
reliable and valid diagnostic criteria (i.e., DSM-IV or NINDCS-ADRDA) such as
the following:
• Loss of memory and one or more additional cognitive
abilities (aphasia, apraxia, agnosia)
•
Insidious onset and gradual progression of symptoms
•
Impairment in social or
occupational functioning
• Cognitive loss documented by neuropsychologic tests
• No physical signs, neuroimaging, or laboratory
evidence of other diseases that can cause dementia (i.e., metabolic
abnormalities, medication or toxin effects, infection, stroke, Parkinson's
disease, subdural hematoma, or tumors)
•There is no definitive imaging or laboratory test for
the diagnosis of dementia.
•NINCDS–ADRDA :National Institute of
Neurological Disorders and Stroke—Alzheimer’s Disease and Related Disorders
Association
•DSM-IV :Diagnostic and Statistical Manual of Mental Disorders
DIFFERENTIAL DIAGNOSIS
•Cancer
(brain tumor, meningeal neoplasia)
•Infection
(AIDS,
neurosyphilis, progressive
multifocal leucoencephalopathy)
•Metabolic
(alcohol, hypothyroidism, B12 deficiency)
•Organ
failure (dialysis
dementia, Wilson's disease)
•Vascular
disorder (chronic
subdural hematoma)
•Depression
WORKUP
•HISTORY & GENERAL
PHYSICAL EXAMINATION:
• Medication use
should always be reviewed for drugs that may cause mental status changes.
•Patients should be
screened for depression, because it can sometimes mimic dementia but also often
occurs as a coexisting condition and should be treated.
•On examination, look
for signs of metabolic disturbance, presence of psychiatric features, or focal
neurologic deficits.
•MENTAL
STATUS TESTING:
•Brief mental status
testing.
•Most commonly used is
the Folstein Mini-Mental Status
Examination (MMSE). A MMSE score <24 (scores range from 0 to 30, with lower
scores reflecting poorer performance) suggests dementia;
•MMSE is not sensitive
enough to detect–
mild dementia,
– dementia in patients with high baseline IQ.– Scores may be spuriously low in patients with limited education, poor motor function, poor language skills, or impaired vision.
– dementia in patients with high baseline IQ.– Scores may be spuriously low in patients with limited education, poor motor function, poor language skills, or impaired vision.
•Attention is usually
preserved until the late stages of AD, so consider alternate diagnoses in
patients who do poorly on tests of attention.
LABORATORY TESTS
•CBC•Serum electrolytes. BUN/creatinine •Glucose , Liver and thyroid function tests•Serum vitamin B12 and methylmalonic acid•Syphilis serology, if high clinical suspicion•Lumbar puncture if history or signs of cancer, infectious process, or when the clinical presentation is unusual (i.e., rapid progression of symptoms)
•EEG if there is history of seizures, episodic confusion, rapid clinical decline, or suspicion of Creutzfeldt-Jakob disease
•Measurement of apolipoprotein E genotyping, CSF tau and amyloid,
•Functional
imaging including positron emission tomography (PET) or scanning proton
emission computed tomography (SPECT) are not routinely indicated
•IMAGING
STUDIES
•CT
scan or MRI to rule out hydrocephalus and mass lesions, including subdural
hematoma.
TREATMENT
•NONPHARMACOLOGIC
THERAPY
•Patient safety,
including risks associated with impaired driving, wandering behavior, leaving
stoves unattended, and accidents, must be addressed with the patient and family
early and appropriate measures implemented.
•Wandering, hoarding
or hiding objects, repetitive questioning, withdrawal, and social
inappropriateness often respond to behavioral therapies.
•ACUTE
GENERAL Rx
–None
–None
•CHRONIC
Rx
1.
Symptomatic treatment of memory disturbance:a. Cholinesterase inhibitors (ChEI): for mild to
moderate AD (MMSE 10-26). Common side effects include nausea, diarrhea, and
anorexia.b. NMDA (N-methyl-D-aspartate )receptor
antagonist: Memantine). for moderate to
severe AD. Common side effects include constipation, dizziness, or headache. Memantine is contraindicated
in patients with renal insufficiency or history of seizures.
2.
Symptomatic treatment of neuropsychiatric and behavioral disturbances:
Depression, agitation, delusions, or hallucinations.